bma flu vaccine funding row sparks warning of costly winter hospital surge

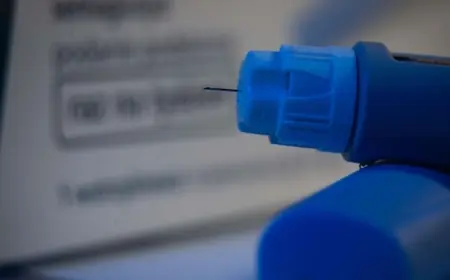
The British Medical Association has sounded an alarm over what it describes as an unsustainable squeeze on payments for flu vaccinations. With reimbursement rates unchanged since 2019 and administration costs rising sharply, some practices are weighing whether to opt out of this autumn’s immunisation programme — a move that health officials warn could push up hospital admissions during the busiest months.
Financial squeeze on GP practices
Clinics that historically ran mass immunisation sessions say the payment structure has not kept pace with inflation and increased operating expenses. The BMA highlights that while vaccine procurement has been negotiated centrally, the fees paid to practices to deliver jabs have effectively been frozen for several years. That gap means staff time, premises overheads and the logistical burden of running clinics are becoming harder to justify financially.
Where practices are contractually obliged to offer vaccinations, managers are exploring cost-cutting measures such as reducing clinic hours or trimming non-clinical staff who support delivery. In other cases, surgeries are considering not signing up at all for the upcoming autumn programme, which would shift the delivery burden to other parts of the health system or leave some at-risk patients with fewer local options.
Risk to winter resilience and patient safety
Public health experts warn that lower uptake of flu vaccines among vulnerable groups — including older people and those with long-term conditions — risks a repeat of previous winters when seasonal respiratory illness added significant pressure to hospitals. A dry financial saving from limiting reimbursements could translate into higher costs later if more people require inpatient care, creating a false economy.
Clinicians point out that preventive immunisation is a relatively low-cost intervention during the autumn but becomes far more expensive once patients are admitted with severe complications. Beyond direct hospital costs, there are intangible impacts: delayed elective care, stretched ambulance response times and increased strain on community services during peak months.
Options for ministers and next steps
Health leaders are urging a review of the reimbursement model ahead of the autumn 2026 campaign. Immediate options include a targeted uplift in practice payments to reflect real-terms cost increases, short-term top-ups for sessions delivered in the community, and flexible commissioning that allows pharmacies and other providers to step in where general practice capacity is limited.
Longer-term reforms could look at simplifying admin processes and introducing outcome-linked incentives to boost coverage among high-risk groups. Any change will need careful planning around supply chains, workforce capacity and clear communications to the public so that local arrangements do not confuse patients seeking their annual jab.
The debate hits at a wider question for health policy: whether upfront investment in prevention is being properly valued against the downstream costs of hospital care. Ministers have been urged to move quickly so that practices can make firm commitments well ahead of the vaccination season, protecting both patients and the wider health service from avoidable winter pressures.
With the risk of higher admissions looming, the coming weeks are likely to set the tone for how the next flu season is managed and whether prevention remains the priority in keeping the most vulnerable safe.