bma flu vaccine funding: doctors warn payment freeze risks winter hospital surge
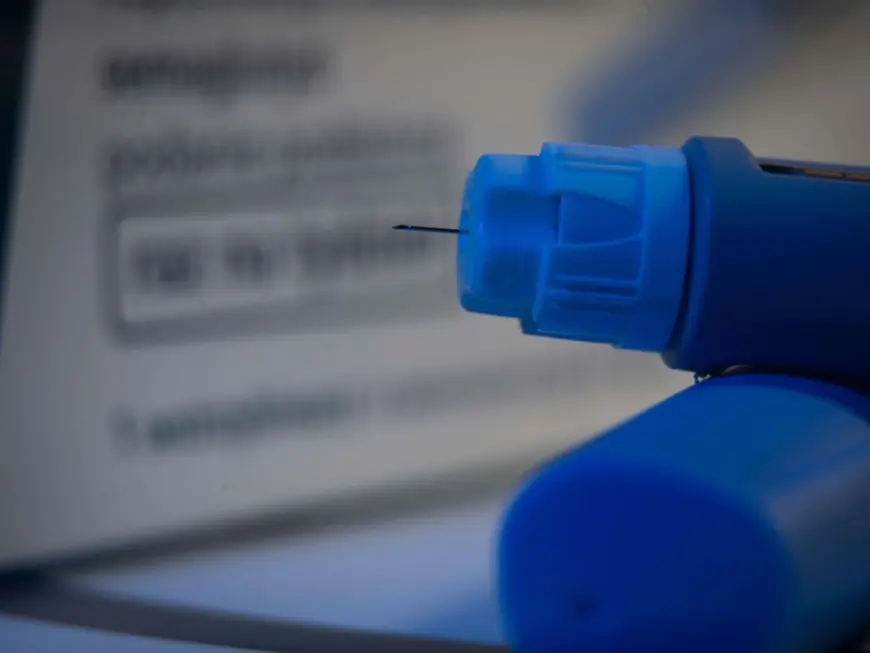
The doctors' trade union has raised the alarm over stagnant payments for seasonal flu vaccinations, saying fees for dispensing jabs have not been adjusted since 2019 while costs of running clinics have climbed. The warning has prompted calls for an urgent review of funding to avoid harm to vulnerable patients and added pressure on hospitals during the cold months.
What the payment squeeze means for GP practices
Clinics that run immunisation programmes face rising overheads from staffing, premises and consumables. With the fee per administered jab unchanged for several years, some surgeries are assessing whether they can continue to offer the service on the same scale—or at all. Practices contractually obliged to deliver vaccinations may respond by reducing clinic hours or trimming support staff, moves that would constrain capacity and slow access for those most at risk.
Healthcare professionals say the shortfall is not just an accounting problem. Running efficient, safe vaccination clinics requires administrative time for recalls and consent, training and oversight to maintain infection control standards, and additional resource when outreach is needed for housebound patients. When reimbursement lags behind those real costs, the service becomes harder to sustain without diverting capacity from other primary-care duties.
Potential consequences for patients and the health system
Public-health experts warn that decreased vaccination uptake among eligible groups could translate quickly into higher rates of influenza in the community, particularly among older adults and people with chronic conditions. That in turn would increase GP consultations, emergency department attendances and hospital admissions during winter—the period when bed capacity is already most constrained.
From a fiscal perspective, any short-term savings achieved by holding down payments could be eclipsed by the downstream costs of additional hospital care and longer inpatient stays. Preventive programmes like seasonal immunisation were designed to smooth winter demand and protect the most vulnerable; undermining them risks reversing hard-won gains in population health and system resilience.
What needs to happen next
Clinics and professional bodies are urging policymakers to review reimbursement levels ahead of the next vaccination campaign and to engage with primary-care leaders on realistic costing. The call extends to ministers responsible for health funding, with appeals to ensure that public-health priorities are matched by sustainable payments for delivery.
Practical steps could include a targeted uplift in fees to reflect current inflationary pressures, streamlined administration for vaccination programmes to reduce practice workload, and earmarked funding for outreach to high-risk, hard-to-reach groups. Without action, the coming autumn campaign faces an avoidable squeeze that could have serious consequences for both patients and the health service.
Healthcare professionals stress that preventive vaccination programmes represent good value when properly resourced. The debate over bma flu vaccine funding is not just a negotiation over tariffs; it is a strategic moment for preserving a frontline defence against a predictable seasonal threat.