Nipah virus outbreak in India 2026 declared contained after two confirmed cases, as Asia tightens airport screening
The Nipah virus is back in headlines in early 2026 after India confirmed two infections in the eastern state of West Bengal and moved quickly to contain what officials described as a limited cluster. The Nipah virus outbreak has also triggered heightened entry screening in parts of Asia, with several governments moving to detect potential imported cases from travelers arriving from India.
India’s health ministry said only two confirmed Nipah virus disease cases have been reported in West Bengal since December 2025 and that extensive tracing and testing of contacts has so far found no additional infections.
What India has said about the Nipah virus outbreak in West Bengal
The Government of India, coordinating with the West Bengal government, said it identified two confirmed cases and launched what it described as comprehensive public health measures in line with established protocols. Officials said 196 contacts linked to the two confirmed cases were identified, traced, monitored, and tested, and that all traced contacts were asymptomatic and tested negative.
The ministry also said enhanced surveillance, laboratory testing, and field investigations were carried out through coordinated efforts by central and state health agencies, and that no additional cases had been detected so far. Further specifics were not immediately available.
While India’s statement aimed to calm speculation, it also underscored why even small Nipah clusters are treated as high priority: the virus can be severe, and hospital-associated spread has been documented in past outbreaks.
Why other countries are screening travelers now
Even when a cluster appears contained, cross-border vigilance is common because Nipah is considered a high-consequence pathogen with a history of serious illness and a lack of widely available licensed vaccines or specific curative treatments. In recent days, multiple governments in Asia have announced stepped-up health checks for arrivals from India, including measures such as temperature screening, health declarations, and enhanced monitoring for symptoms consistent with acute infection.
These steps are designed to reduce the risk of a delayed diagnosis in someone who becomes ill after travel, especially if that person seeks care in a busy hospital setting where close contact can amplify transmission. Some specifics have not been publicly clarified, including how long enhanced screening will remain in effect and whether it will be expanded to additional routes.
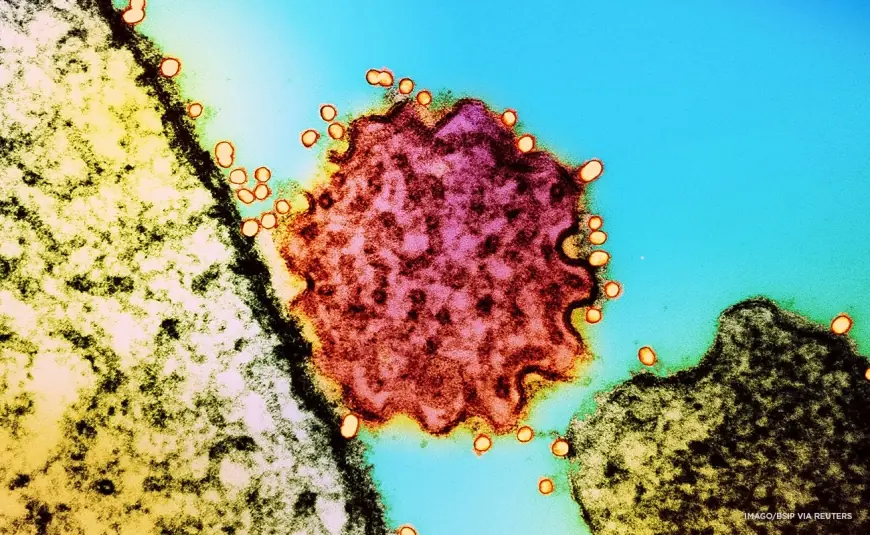
How Nipah spreads and why hospitals focus on contact tracing
Nipah is a zoonotic virus, meaning it can spill over from animals to humans. Fruit bats are widely recognized as the natural reservoir, and human infections have been linked to exposure pathways that include contaminated food or drink, including fruit or sap contaminated by bat saliva or urine. In parts of South Asia, raw date palm sap has been repeatedly cited as a risk pathway when collected overnight and consumed without processing.
Human-to-human transmission can occur, typically through close contact with an infected person’s bodily fluids or contaminated tissues. That is why hospitals and household caregivers often become central to containment strategies: when a suspected case emerges, health teams isolate the patient, identify close contacts, monitor them for symptoms through the incubation window, and test as needed. Infection prevention controls in healthcare settings, along with careful use of personal protective equipment, are treated as critical to stopping onward spread.
In plain terms, containment depends on speed and precision: isolate the case, map exposure, test contacts, and keep surveillance high enough to catch any secondary infections early.
What this means for communities, healthcare workers, and travelers
The India Nipah virus outbreak response has immediate impacts across several groups. Healthcare workers face heightened risk and stricter infection control demands when even a small cluster is detected, including staffing pressures from isolation protocols and monitoring requirements. Patients and families can feel the effects through tightened hospital access rules, increased screening at facilities, and delays caused by precautionary triage steps.
Travelers and airport staff are another major stakeholder group. Enhanced screening can add time and friction to international arrivals, while also raising anxiety for people who have routine fevers unrelated to Nipah. Businesses linked to travel may experience disruption if passenger confidence drops, even when public health authorities describe the broader risk as low.
Historically, Nipah outbreaks in India have appeared as localized clusters, notably in Kerala in recent years, with West Bengal previously affected in earlier decades. That history is part of why officials move quickly even when case counts are small.
The next verifiable milestone is expected to be additional updates from India’s health authorities as ongoing surveillance and contact monitoring continue, including any formal health briefing that confirms no new cases have emerged over the monitoring period.