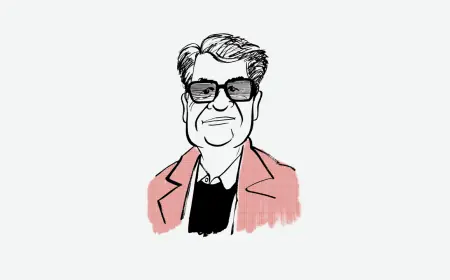
Grassley Report Uncovers UnitedHealth’s Manipulation of Medicare Advantage Risk Adjustments

A recent report released by Senator Chuck Grassley (R-Iowa) brings to light serious allegations against UnitedHealth Group (UHG). The report alleges that UHG manipulated the Medicare Advantage (MA) system, exploiting risk adjustments for financial gain. Grassley, a prominent figure in Congress and currently chair of the Senate Judiciary Committee, based his findings on a detailed review of over 50,000 UHG documents.
Overview of the Allegations
The report, titled “How UnitedHealth Group Puts the Risk in Medicare Advantage Risk Adjustment,” reveals how UHG may have turned risk adjustment into a profitable enterprise. It claims that UHG has employed various resources and strategies to inflate the number of diagnostic codes it reports. This manipulation allows the company to secure higher payments from the Centers for Medicare and Medicaid Services (CMS) compared to its competitors.
Background on Medicare Advantage
- More than half of Medicare beneficiaries are enrolled in Medicare Part C.
- CMS reimburses Medicare Advantage Organizations (MAOs) based on monthly risk-adjusted amounts, reflecting the health status of enrollees.
- MAOs receive higher payments for sicker patients needing more healthcare services.
With a higher number of diagnoses, MAOs like UHG can boost their risk scores, resulting in increased funding. However, this system is under scrutiny for potentially incentivizing excessive coding that does not align with CMS guidelines.
Critical Findings from the Report
- Exploitation of Risk Adjustment: UHG reportedly utilizes aggressive tactics to maximize its risk adjustment scores.
- Utilization of Specialized Workforce: UHG’s significant resources include nurse practitioners and coders, who help capture more diagnoses.
UHG’s Approaches to Risk Adjustment
Senator Grassley’s report highlights two key practices employed by UHG:
- In-Home Health Risk Assessments (HRAs): UHG hires nurse practitioners to evaluate patients’ health in their homes, increasing the capture of diagnoses.
- Data Analytics and AI: The company leverages advanced operations to identify emerging opportunities for diagnosis coding.
Specific Examples of Coding Practices
The report outlines several controversial diagnostic practices by UHG that raise ethical questions:
- Opioid Dependence: UHG advises that patients prescribed opioids can be diagnosed with dependence without exhibiting withdrawal symptoms.
- Alcohol Use Disorder: The company’s guidelines allow for diagnoses based on screening tools, despite contrasting with established diagnostic criteria.
- Dementia Diagnoses: UHG suggests that a diagnosis can be made using minimal assessments, which could lead to inaccurate coding.
Grassley’s Ongoing Oversight
Senator Grassley has a long history of advocating for proper Medicare practices. Since the advent of Medicare Advantage, he has monitored its implementation closely. In 2015, he urged CMS and the Department of Justice to recover improper payments within the program.
The report concludes with Grassley’s call for transparent risk adjustment processes. As taxpayer dollars are increasingly funneled into Medicare Advantage, Congress must ensure these funds are utilized effectively and ethically.