Kaiser Permanente Settles Medicare Overbilling Claims for $556 Million
Kaiser Permanente has agreed to a historic settlement of $556 million with the federal government and two whistleblowers. This agreement resolves accusations of fraudulent overbilling related to its Medicare Advantage plans. The lawsuits, dating back over a decade, alleged that Kaiser inflated patient diagnoses to secure higher federal payments.
Kaiser Permanente’s Overbilling Allegations
The settlement represents the largest financial figure recorded in a Medicare Advantage case. Medicare Advantage plans, which have grown controversial, now cover over half of the eligible individuals in the United States. The issues surrounding these plans have garnered significant scrutiny from lawmakers and health care experts, especially regarding payment system abuses.
Key Details of the Settlement
- Amount: $556 million
- Duration of Lawsuits: Filed over 12 years ago
- Government Estimate: Kaiser allegedly received $1 billion from 2009 to 2018 due to inflated diagnoses.
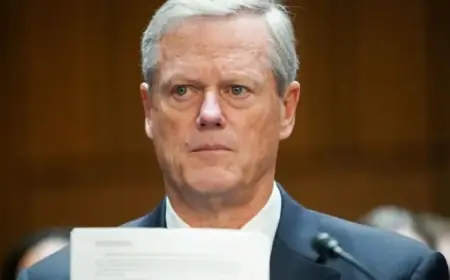
U.S. Attorney Craig H. Missakian emphasized the importance of protecting taxpayer interests from fraud and abuse within the Medicare program. He stated, “Medicare Advantage must serve patients’ needs, not corporate profits.” Although Kaiser issued a statement saying the suit was not about the quality of care, they did not admit any wrongdoing.
Falsified Diagnoses and Pressure Tactics
The lawsuits described practices where Kaiser executives pressured doctors to add more patient diagnoses weeks after treatment. This practice aimed to increase revenues through bonus funds from higher government payouts for sicker patients. Meetings attended by doctors, allegedly funded by Kaiser, focused on coding visits with additional diagnoses that yielded financial benefits.
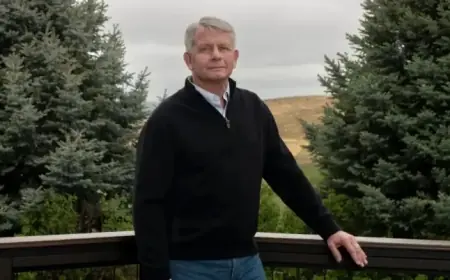
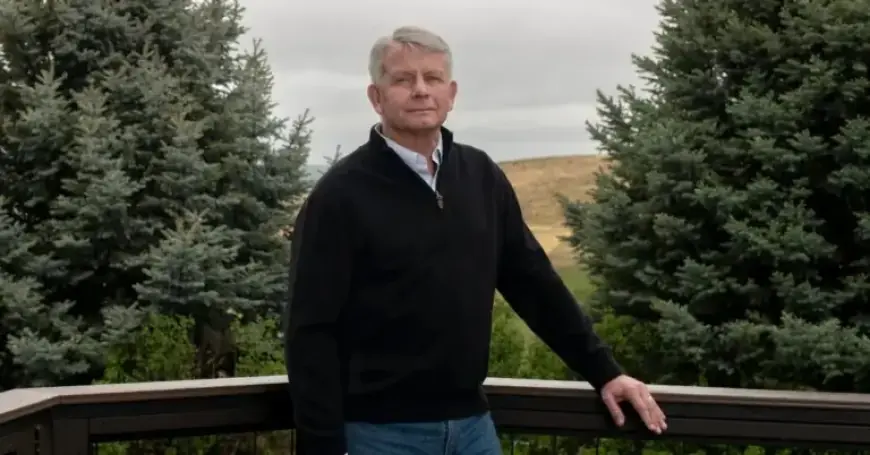
Whistleblower Insights
Dr. James Taylor, one of the whistleblowers and a former Kaiser physician, highlighted the pressure to identify additional diagnoses. He referred to the strategy as a “cash monster” hungry for profits. His actions reflect a significant backlash against fraudulent practices in the healthcare sector.
Industry-Wide Implications
Audits and investigations have shown that similar coding fraud exists across the healthcare industry. Five out of the ten largest insurers have faced federal lawsuits or settlements regarding such practices. Recently, Senator Chuck Grassley has accused UnitedHealth Group of similar overbilling tactics.
Government Response and Future Actions
The Justice Department continues to focus on Medicare Advantage oversight, having recently made settlements with Independent Health and Cigna for similar offenses. The Biden administration is seeking to reduce overbilling by adjusting payment processes, although progress has been slow due to industry resistance.
Dr. Taylor expressed his commitment to justice, stating he plans to donate most of his settlement to charity. He emphasized the importance of accountability over financial compensation, saying, “Knowing people understand the wrongs that were committed makes me feel better.”